cutting-edge Brain & Spine Treatments we offer
MinImally invasive spine surgery
Lumbar Microdiscectomy
A Lumbar Microdiscectomy is a minimally invasive surgery to remove a herniated or degenerative disc from the lower back. A small, one-inch incision is made in the lower back and the back muscles are separated to reach the damaged disc by first removing the lamina, or “bone roof.” Then, a special tool is used to remove the piece of the disc that is compressing or “pinching” the nerve causing pain.
Lumbar Laminectomy
A Lumbar Laminectomy procedure decompresses the spinal cord and nerves by removing a portion of the lamina, or “bone roof,” that covers them. Creating more space in the spinal canal allows the spinal cord and nerves to move more freely, relieving chronic pain, numbness and weakness of the appendages caused by spinal stenosis.
Lumbar Foraminotomy
A Lumbar Foraminotomy is a surgery to open the tunnels in the vertebrae where the nerves exit off of the main spinal cord. This technique is used to decompress a painful nerve. The incision is made through the lower back and the intervertebral foramen is widened. Blockages such as bone spurs and disc fragments are removed to provide space for the nerves.
Lumbar Spinal Fusion
There are several types of spinal fusions. Some of the different fusion surgeries we perform are: an Anterior Lumbar Interbody Fusion (ALIF), an Extreme Lateral Lumbar Interbody Fusion (XLIF), a Posterior Lumbar Interbody Fusion (PLIF) and a Transforaminal Lumbar Interbody Fusion (TLIF). All can be done through a minimally invasive technique that alleviates disc-related discomfort and structural deformity in the lower back by joining two or more bones to stabilize the spine and prevent painful movement.
In an ALIF procedure, an incision is made at the lower abdomen and the damaged disc is removed. It is replaced with a bone graft to correct spacing and relieve nerve pinching. An XLIF procedure is executed through a small incision at the side of the waist. The damaged disc is removed and replaced with a bone graft to correct spacing between vertebrae. In a TLIF procedure, an incision is made posterior and the damaged disc is removed and replaced with an implant packed with bone graft. Each of these surgeries may require additional placement of rods and screws for added stabilization.
SI Joint Fusion
The iTORQ Implant System is designed to stabilize and fuse the SI joint. The iTORQ procedure involves inserting typically a titanium screw across the sacroiliac joint to maximize SI joint stability, reduce pain, and improve function. The procedure is done through a small one-inch incision and takes about an hour. SI joint treatment using the patented design of the iTORQ implant has been clinically evaluated more than any other SI joint fusion procedure.
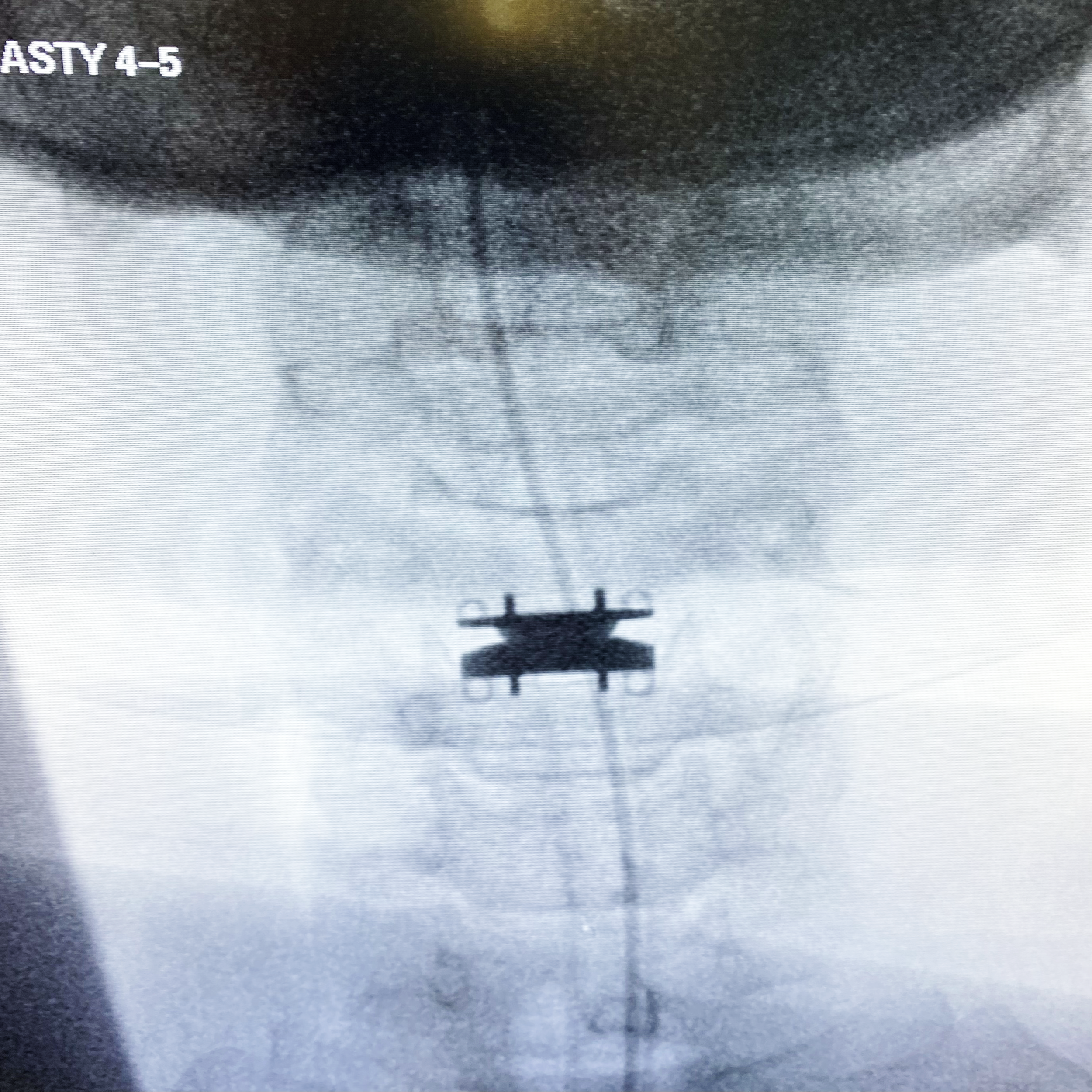
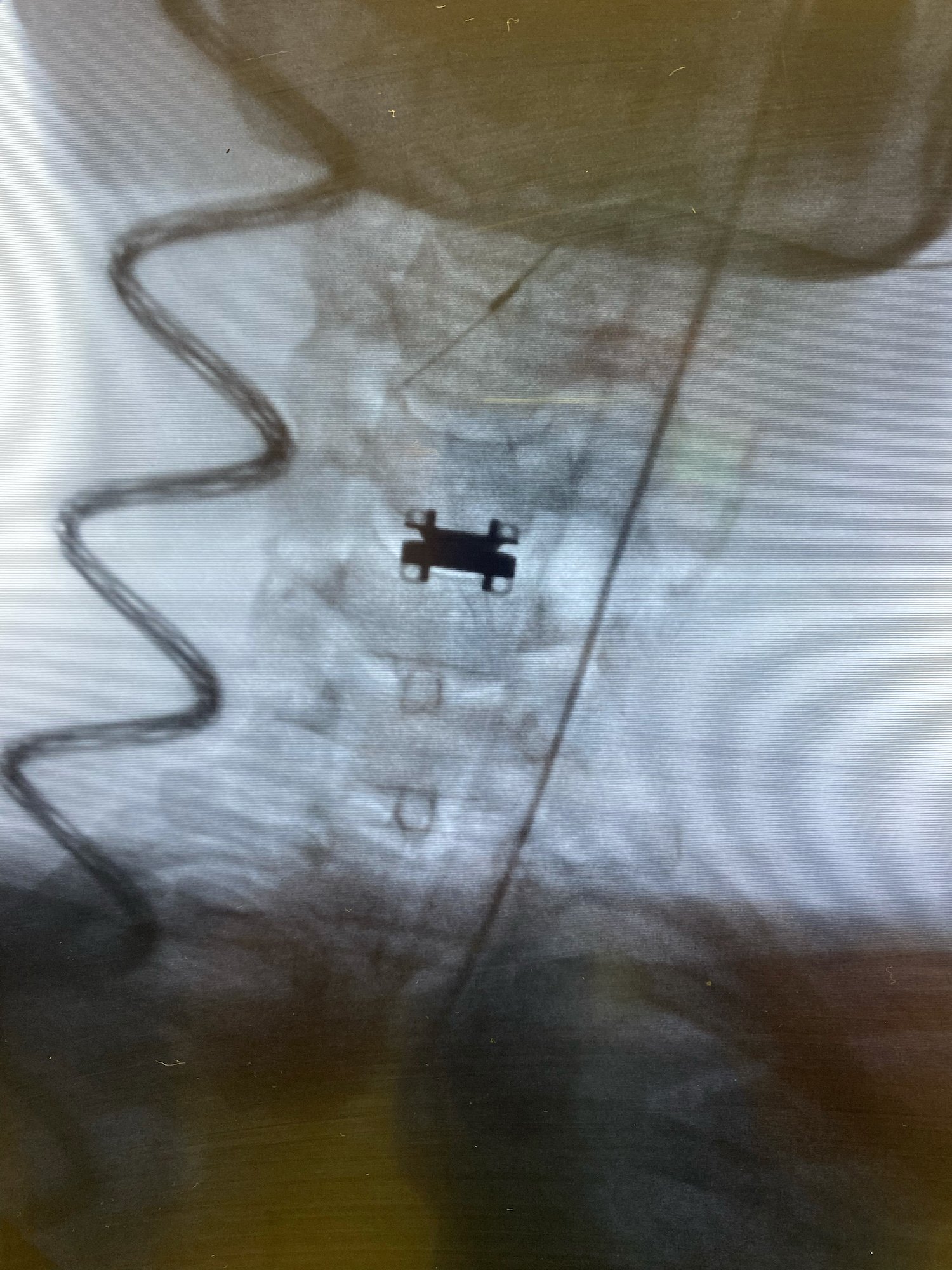
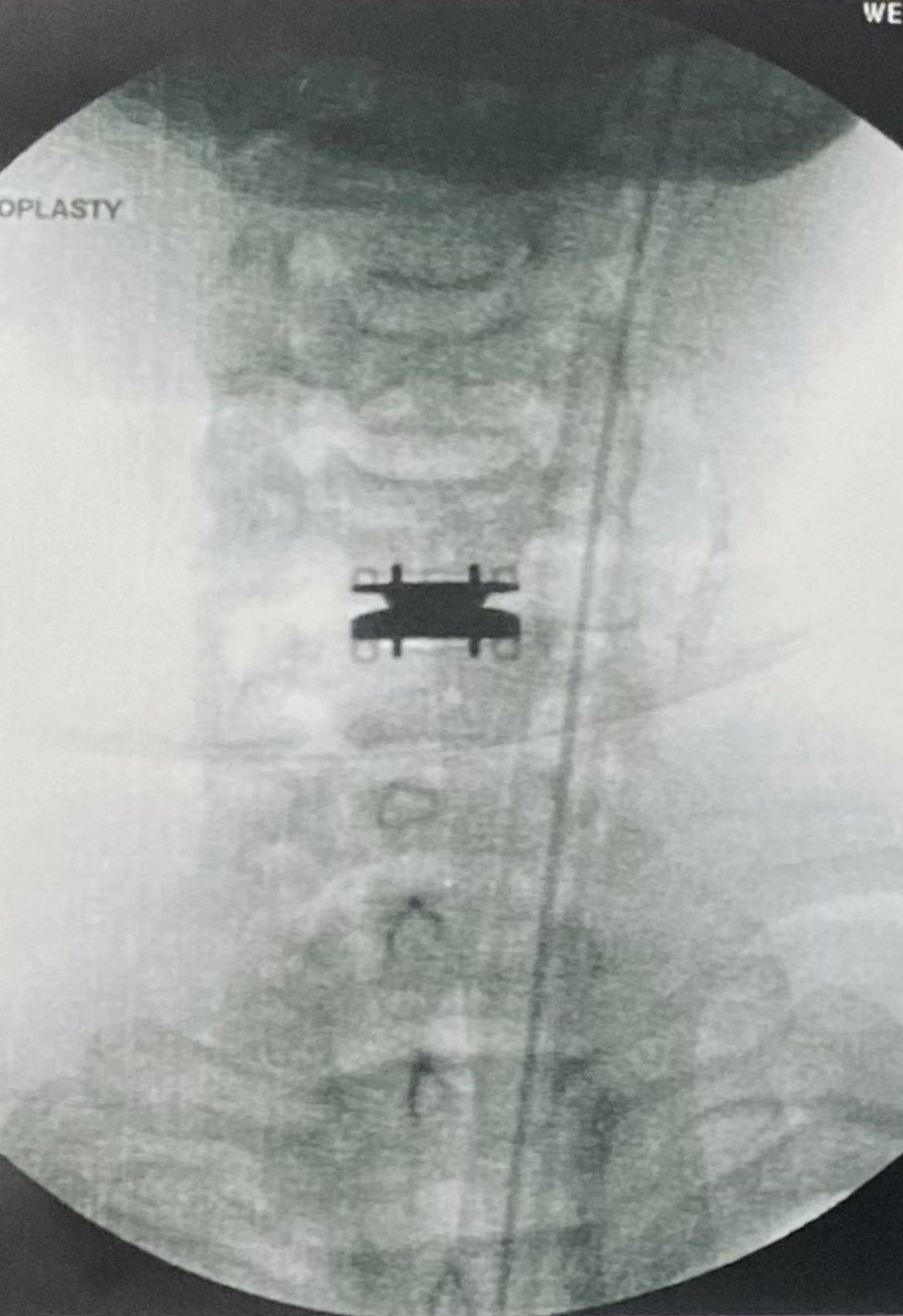
Disc Replacement (Arthroplasty)
A Disc Replacement procedure removes the damaged disc causing pain and replaces it with an artificial one. The artificial disc is inserted in the open space between the vertebrae to decompress nerves and maintain the spine’s natural movement.
Anterior Cervical Discectomy & Fusion
The Anterior Cervical Discectomy and Fusion is conducted through a small incision in the front of the neck to remove a herniated or degenerative disc and replace it with a bone graft. The procedure alleviates pinched nerves causing neck or arm pain.
Cervical Posterior Foraminotomy
A Cervical Posterior Foraminotomy is a minimally invasive procedure to alleviate pain and muscle weakness caused by a pinched nerve. The surgery accesses the nerve root through a small incision in the neck and cuts away the bone to expose the root. If compression is caused by the disc, it is removed to relieve pressure.
Cervical Posterior Facet Joint Fusion
Pain caused by facet joint syndrome or spinal arthritis is treated with a Cervical Posterior Facet Joint Fusion. Deterioration of the joints is caused by loss of synovial fluid, which lubricates the joints and discs, creating friction. In the procedure, two or more vertebrae are fused together to prevent the joint movement causing pain.
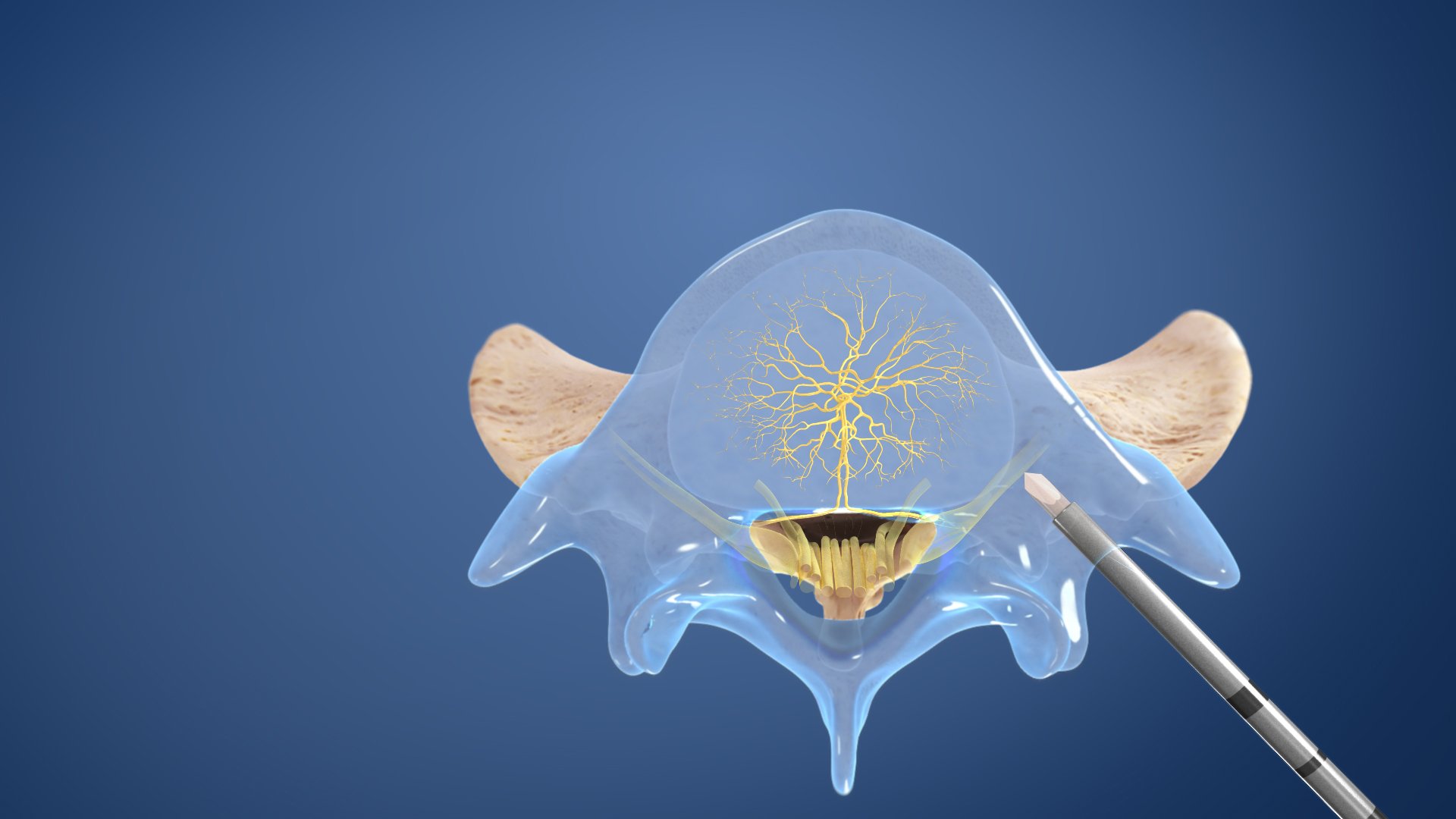
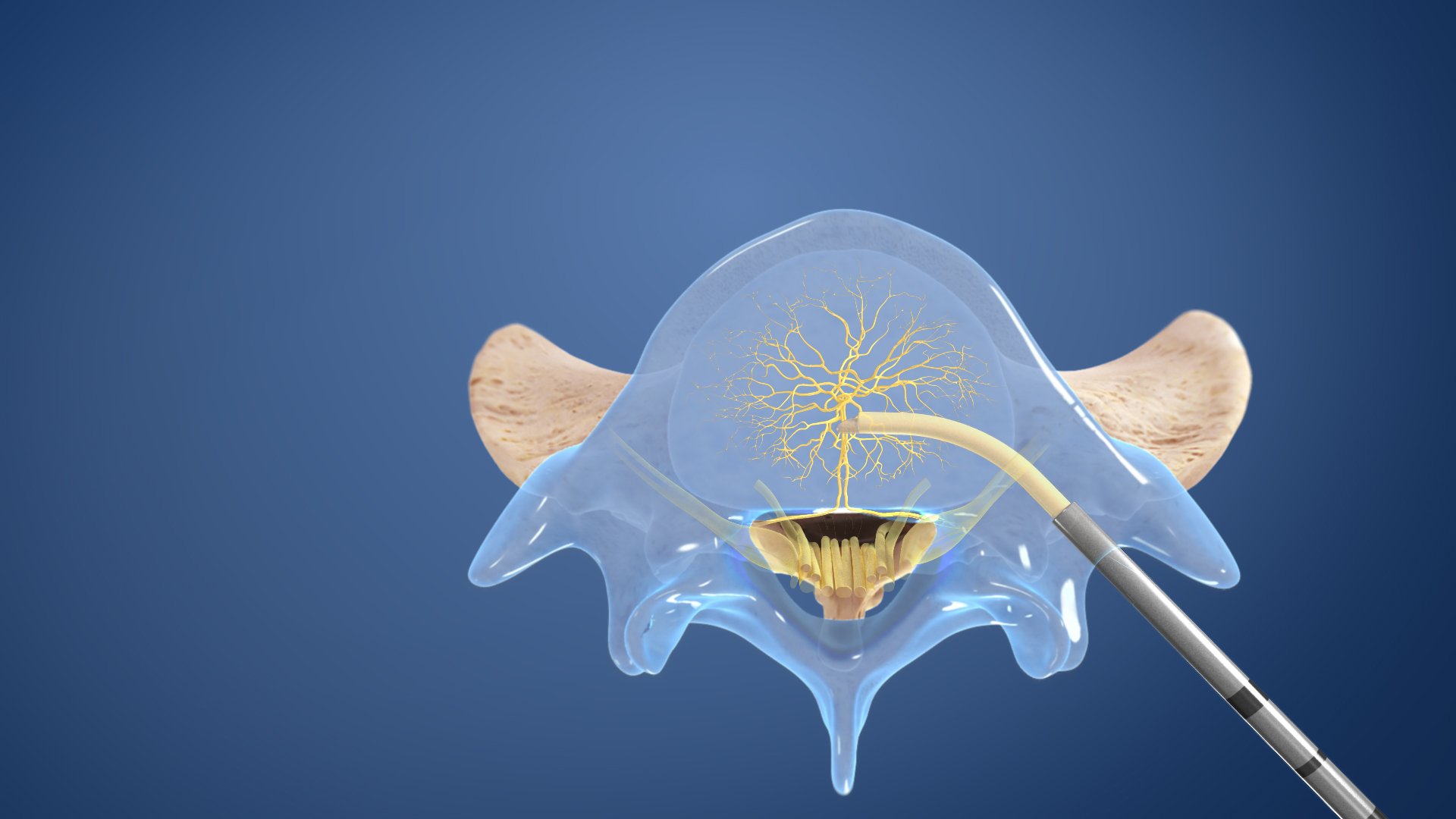
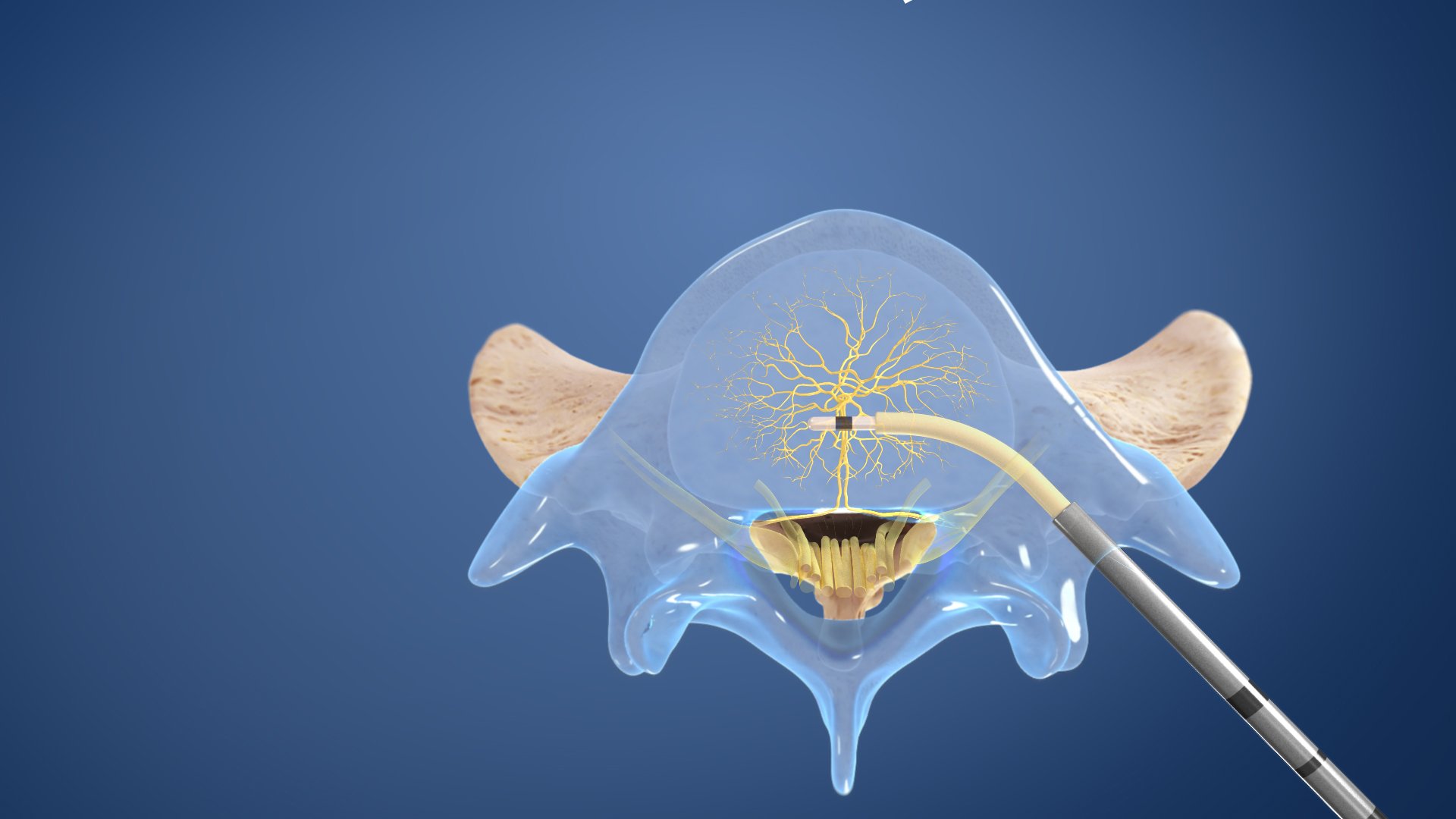
Spinal Cord Stimulator Implant
A Spinal Cord Stimulator is an implant that emits low-level electricity to the spinal cord to alleviate pain. In the procedure, the device’s electrodes are placed between the spinal cord and the vertebrae and its generator is placed under the skin. Patients can control a remote to activate the stimulator when they feel pain.
Complex spinal tumor resection
peripheral tumor resection
neurosurgery
Minimally Invasive Tumor Resection
In cases where a Minimally Invasive Tumor Resection is ideal, the goal is to fully remove the tumor. The tumor, along with a small amount of healthy tissue surrounding it, is completely removed when possible. The procedure is performed through a “keyhole” incision utilizing robotic navigation assistance for a minimally invasive approach. Depending on the patient, Tumor Resection may be recommended prior to or following radiation therapy.
Open Tumor Resection
In cases where a Minimally Invasive Tumor Resection is not ideal, an Open Tumor Resection is performed. The goal of the procedure is to achieve a gross total resection of the tumor by removing the tumor until a rim of healthy margin of brain tissue is seen. The incision is large enough to allow the surgeon to see inside the affected area.
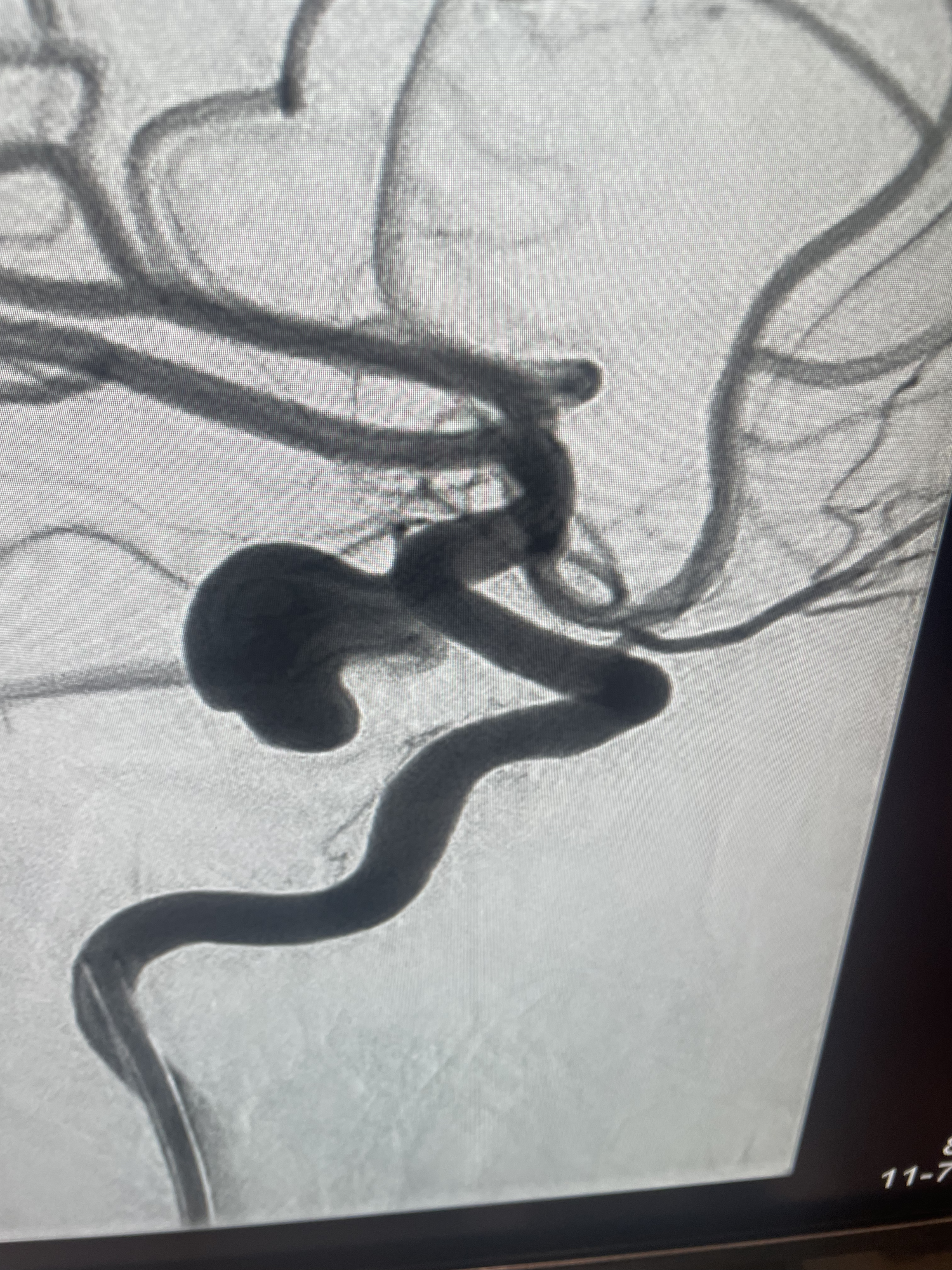
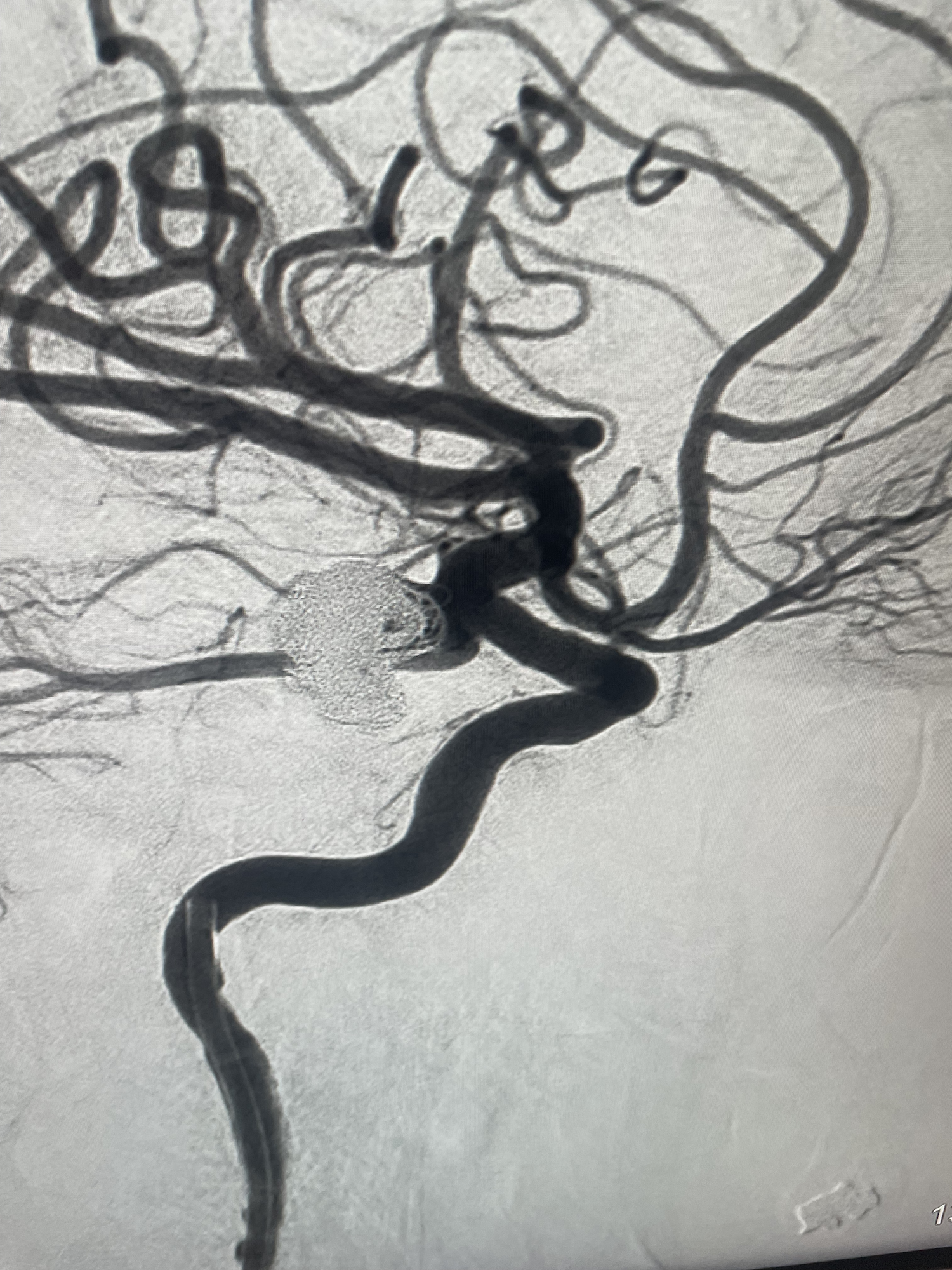
Aneurysm Clipping and Coiling
A brain aneurysm is a balloon-like bulge or the weakening of an artery wall, which can rupture and result in life-threatening bleeding in the area surrounding the brain. Aneurysms can be treated by clipping and coiling to prevent further growth. When clipping an aneurysm, a craniotomy is performed wherein the skull is opened and a small clip is placed around the neck of the aneurysm to stop blood from entering the aneurysm. When coiling an aneurysm, this procedure is done as an “endovascular approach” much similar to a cardiac catheterization. The surgeon can use a catheter to deploy coils into the aneurysm, which fills it up and prevents it from getting larger.
Endovascular Cerebral Artery Stenting
An Endovascular Cerebral Artery Stenting procedure is performed inside the artery through a thin tube called a catheter. A tiny incision is made in the blood vessel (typically in the groin area) and the steerable catheter is inserted. The blood stream guides the catheter to the brain, where a mesh stent is placed to promote clotting, essentially closing off the artery.
Ventriculoperitoneal Shunt Placement
A Ventriculoperitoneal Shunt Placement is a surgical procedure that places a medical device called a shunt, which is a small hole or passage, in the ventricle to relieve pressure caused by fluid build-up. Oftentimes, a ventriculoperitoneal shunt is used to treat hydrocephalus wherein cerebrospinal fluid builds up in the ventricles, expanding the affected area and causing damage that may lead to symptoms of mild dementia, cognitive delays, shuffled gait or incontinence.
Craniectomy/Craniotomy
Both a Craniectomy and a Craniotomy involve removing a small or large portion of the skull, depending on the issue being treated. A Craniectomy is simply removing a part of the skull to decompress the swollen brain. It is usually performed on patients who have experienced traumatic brain injury and/or have swelling of the brain. A Craniotomy also cuts away a portion of the skull to access the brain for the treatment of tumors, hematomas, aneurysms and several other possible conditions. The bone flap is typically replaced upon recovery using plates and screws.
Cranioplasty
A Cranioplasty is performed to treat a deformity of the skull caused by trauma, surgical complications or abnormalities present from birth. An incision is made to access the skull, where the condition of the bone (or lack of bone) will determine the strategy. If the skull is intact, titanium plates and screws can be used to shape and reposition the bone. If a replacement for the portion of skull is deemed necessary, a graft or synthetic material is affixed to the surrounding skull bone using titanium plates and screws. The strategy and materials used are typically decided upon prior to surgery.
Microvascular Decompression
A Microvascular Decompression surgery is performed to treat trigeminal neuralgia, glossopharyngeal neuralgia and hemifacial spasm, which cause compression on a cranial nerve. In the procedure, a craniotomy is conducted to access the nerve and a sponge is inserted to alleviate the pressure of the imposing artery or vein.
Chiari Malformation Repair
Chiari Malformation occurs when the cerebellar tonsil, or the lower section of the brain, herniates, or squeezes through the skull, protruding into the spinal canal. The imposing tissue presses against the brainstem, blocking cerebrospinal fluid from flowing normally. A repair is made to expand the foramen magnum, allowing enough space for the brain. Bone from the back of the skull is removed and the dura covering the tonsils is opened up. A patch is placed to accommodate the expansion, which will relieve the pressure and restore cerebrospinal fluid flow going forward.
Stereotactic Radiosurgery Cyberknife
The Cyberknife method of Stereotactic Radiosurgery is a noninvasive approach where a robotic delivery system deploys radiation to treat tumors and other conditions. In a Stereotactic Radiosurgery Cyberknife procedure, a precise distribution of high-dose radiation specifically targets diseased tissue, while avoiding the surrounding healthy tissue.
Ventriculoscopy
minimally invasive procedures
Facet Injections
A Facet Injection is a medicine mixture injected into the facet joint using X-ray guidance. Facet joints are the small joints located between each spinal segment that promote stability and guide movement. Arthritis, injury or stresses can cause pain in the facet joint.
Trigger Point Injections
When a muscle does not relax, a painful area containing a trigger point may be formed under the skin. Trigger points, or knots of muscle, cause pain to the immediate area surrounding it by irritating the nerves and can also cause the pain to be felt in another part of the body. In a trigger point injection, a small needle is inserted at the trigger point. A local anesthetic or saline is injected, which may include a corticosteroid. After the injection, the trigger point becomes inactive and pain is alleviated.
Spinal Cord Stimulator Trial
A Spinal Cord Stimulator Trial measures the effectiveness of spinal cord stimulator to treat chronic pain. The response varies between patients, which is the reasoning behind a trial period. For seven days, the stimulator is temporarily inserted and programmed for neuromodulation, blocking nerve and pain signals. During the procedure, a needle is inserted into the epidural space at the base of the spine. One or several leads are threaded through the needle, up into the target level, typically several inches above the needle. The leads are connected to the stimulator, which is secured to the patient’s skin and controlled by a handheld device. If the trial is a success, a Spinal Cord Stimulator is permanently implanted using a similar technique as the trial, however, the battery pack is surgically implanted along the posterior hip region.
Kyphoplasty/Vertebroplasty
Both Kyphoplasty and Vertebroplasty procedures correct injury caused by fractured vertebrae. In a Kyphoplasty, a balloon catheter is used to help position bone cement restoring the position of the broken vertebra. The balloon catheter is inserted into the damaged vertebra with X-ray guidance and is then inflated with liquid. As the balloon is filled, the proper positioning of the collapsed vertebra can be restored and abnormal wedging can also be corrected. Once the balloon is fully inflated and the vertebra is repositioned, the balloon is then deflated and the space restored is filled with thick bone cement under lower pressure to maintain the positioning.
A Vertebroplasty differs in that a balloon is not used and the bone cement is injected directly through a thin needle cannula into the vertebra. The procedure uses more pressure and the material is placed directly into the site of the fracture without first manipulating its positioning. When the bone cement hardens, it stabilizes the bone fragments from the fracture, binding them together to remain in place.
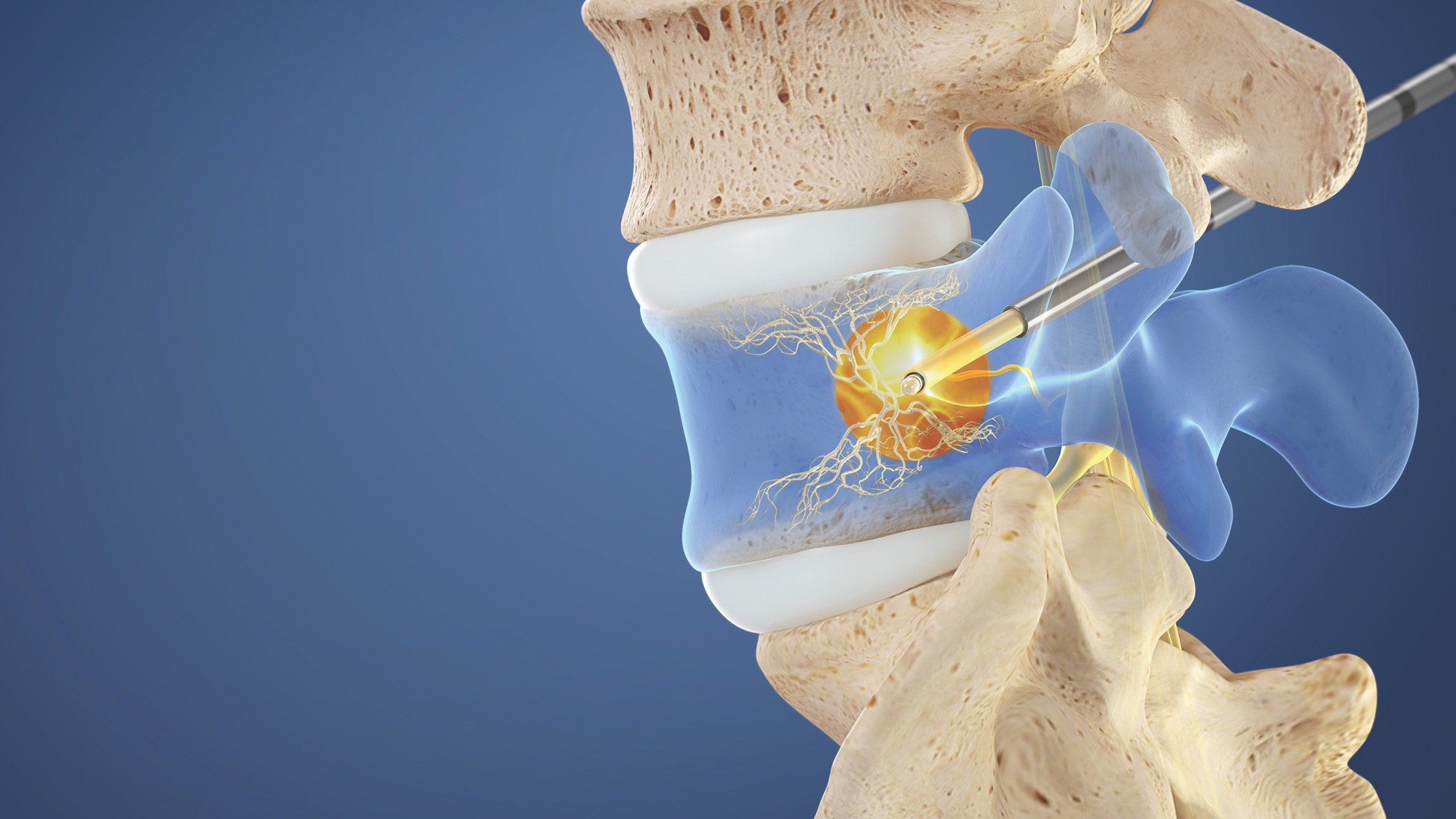
Intracept® Procedure
The Intracept® Procedure is a minimally invasive treatment that stops pain signals from the Basivertebral Nerve using radiofrequency energy (heat). The procedure can be performed within the same day, implant-free, preserving future treatment options. It is performed through two small one-centimeter incisions per every two vertebrae.
muscle biopsy
nerve biopsy